Clinical Workflows Under Pressure: Innovation in Digital Healthcare Platforms 2025
By PAGE Editor
Breaking the Bottlenecks in Clinical Workflows: Real Fixes with Digital Healthcare Platforms
The healthcare environment does not wait. Emergencies arise unexpectedly, patients move across departments, and judgments are frequently made in minutes. However, outmoded Clinical Workflows stifle this urgency by causing fragmented communication, unconnected systems, and repetitive tasks that drain care teams' time and energy. What is the outcome? Delays in diagnosis, professional exhaustion, and avoidable hazards to patients.
The pressure to adapt is not voluntary. Clinical teams are expecting more efficient care delivery pathways that are free of superfluous documentation, ambiguous handoffs, and incompatible equipment.
The difficulty is genuine, but so is the answer.
Where Most Systems Break Down
Many healthcare systems were constructed as silos. Radiology systems do not communicate with pharmaceutical instruments. Nursing paperwork is not available to physicians in real-time. Care transitions are fraught with phone calls, voicemails, and missed follow-ups. Even hospitals that have invested in EHRs and portals struggle to get uniform visibility and smooth activities.
Workflow Gaps That Cost Lives
Data fragmentation: Clinical data is frequently kept across several systems that do not communicate in the same language.
Redundant tasks: Providers must continually enter the same data, which takes up hours of their day.
Care handoff confusion: Delays arise because different teams may not always agree on a patient's condition.
Alert fatigue: Clinicians who get too many pointless notifications become desensitized and run the danger of overlooking actual warning signs.
Moving From Chaos to Clarity
It takes more than just making interface adjustments to redesign healthcare workflows. Rebuilding the whole care journey with precision, speed, and teamwork at its center is the goal.
It is now essential for advancement to have a next-generation digital health platform. These systems push automation in jobs that should not require human labor anymore, deliver real-time insights into therapeutic environments, and integrate heterogeneous data.
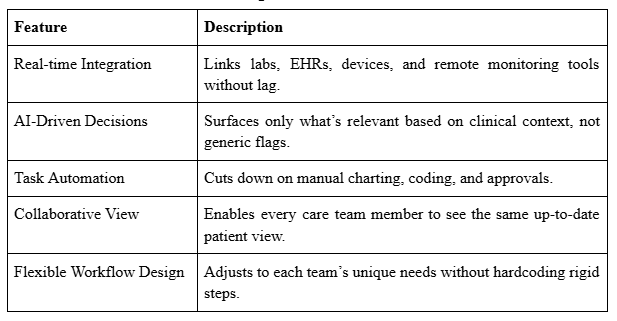
Characteristics of a Functional Digital Health Platform
Why Broken Workflows Hurt More Than Just Operations
Disjointed processes hit three places hardest:
1. Provider Burnout
When clinical time is consumed by data searches, paperwork, and inefficient software, emotional weariness ensues. Burnout is an indication of bad design, not a side effect.
2. Delayed Clinical Decisions
Error risk rises with hidden alarms or lagging diagnostics. Clear, real-time information flow is essential for prompt intervention.
3. Patient Outcomes
Ineffective communication or slow updates to care plans lead to difficulties, needless hospitalizations, or worse.
What Real Workflow Innovation Looks Like
Increasing the number of dashboards is not a sign of progress in digital healthcare innovation. It entails removing blind areas. Solutions must:
Designed with fluidity and quickness in mind.
Use AI and NLP to forecast care shortfalls.
Encourage value-based objectives (improving quality scores, preventing readmissions).
Reduce the number of clicks and tedious manual inputs
Reducing friction is the aim, not adding tools.
Building Workflows Around the Patient, Not the System
Patients must be at the center of a contemporary digital health platform. This implies:
The same real-time insights are available to all members of the care team.
The flow of care incorporates risk ratings and predictive analytics.
Transitions, follow-ups, and social factors are automatic triggers rather than afterthoughts.
Actionable Change at the Clinical Level
Not every company can completely revamp its IT stack in the future. However, wise, effective actions may begin right away:
1. Standardize Data Inputs
Reduce duplication by organizing incoming data into a common format that facilitates actionable insights.
2. Identify Workflow Delays
Reassign accountability or automate triggers when clinical actions, such as order approvals or referral follow-through, stall.
3. Reduce Unnecessary Clicks
Examine the number of steps required for a physician to record a note or request a test. Next, simplify it.
4. Use AI to Surface What Matters
Do not make too much noise for the suppliers. Allow NLP tools to only send out high-risk, urgent notifications.
What the Future Demands
Innovation in digital healthcare will continue to pick up speed. Clinging to old systems will force providers and organizations to lag behind, not because of cost, but because delays cost lives, team morale, and the quality of treatment.
Tomorrow’s Standard, Today
You now anticipate things that were formerly deemed advanced, such as integrated SDOH tracking or predictive care. Additionally, population-level care insights and real-time intervention will soon be standard practice.
Takeaway
Now is the moment to reconsider clinical workflows. That does not imply more layers, lengthier procedures, or larger software. It entails alignment, clarity, and the elimination of superfluous elements.
Every second saved, every duplication avoided, and every smooth handoff is a patient victory rather than a production gain.
Why Persivia Stands Out
Persivia is aware of the vital signs in healthcare environments. Its products represent the future of connected, outcomes-focused care delivery with their AI-driven automation, smooth integration, and real-time care insights. Persivia's Digital Health Platforms help healthcare organizations turn their vision into clinical action, whether your goal is to improve clinician experience, minimize readmissions, or close care gaps.
HOW DO YOU FEEL ABOUT FASHION?
COMMENT OR TAKE OUR PAGE READER SURVEY
Featured






Rain begins to fall, and most homeowners retreat indoors, trusting their gutters to handle the deluge.